
Go to:

TOC
Prev
Next
|
T-Cell Lymphomas
T-CELL lymphomas are the great white whales of hematopathology because:
- They are uncommon compared to B-cell lymphomas, comprising only 15% of lymphomas in the United States (they are much more frequent in parts of Asia).
- In cases that are morphologically not clearly malignant, there is no easy way to
assay their clonality comparable to testing for monotypic light chain expression in B-cell cases.
- The Working Formulation classification is even less successful than with B-cell lymphomas in defining distinct biological or clinical entities.
- Compared to B-cell syndromes, there are more T-cell syndromes that shade stealthily from atypical but non-clonal proliferations into clonal malignancies--angioimmunoblastic lymphadenopathy, lymphomatoid papulosis, and others.
In cases of morphologically uncertain malignancy, two ancillary methods of establishing
clonality are available. The first is to use molecular techniques such as Southern blotting
to look for a unique, clonal rearrangment of the T-cell receptor gene, which in benign populations exhibits a
slightly different rearrangement in each cell. A second method is to demonstrate
immunophenotypically that the suspicious population of T-cells uniformly fails to express
a pan-T-cell antigen such as CD2, CD3, CD5, or CD7.
Lymphoblastic Lymphomas
Some T-cell lymphomas are malignancies of primitive lymphoid progenitors from the thymus.
Called lymphoblastic lymphomas, they are composed of T-cell blasts that usually contain terminal deoxynucleotidyl transferase. This is an enzyme necessary for the rearrangement of the T-cell receptor, an event marking a T-cell's commitment to immunologic adulthood (think Bar Mitzvah or Confirmation). Lymphoblastic lymphomas have already been discussed in the previous section.
Peripheral (or Post-Thymic) T-Cell Lymphomas (PTCL)
PTCLs derive from T-cells that have fled the
horrors of generation
in the central, thymic nursery to join the ranks of the mature immune system billeted in the peripheral lymph nodes. Some entities in this category have distinct morphologic, immunophenotypic, or other qualities. Such lymphomas include:
- T-cell chronic lymphocytic leukemia (large granular lymphocyte leukemia of either T-cell CD8+ subtype or natural killer cell subtype)
- Cutaneous T-cell lymphoma (mycosis fungoides/Sezary syndrome)
- Anaplastic large cell lymphoma, T-cell type
- Intestinal T-cell lymphoma (enteropathy associated)
- Adult T-cell leukemia/lymphoma
- Angioimmunoblastic lymphadenopathy with dysproteinemia-like T-cell lymphoma
- Angiocentric lymphomas, so-called "T-cell" type
Other PTCLs do not nest comfortably in their own pigeon holes and are lumped together as peripheral T-cell lymphomas not otherwise specified (PTCL-NOS).
Although PTCLs are an extremely heterogeneous collection, they tend generally to be aggressive diseases. By the Working Formulation, most of them would fit the diffuse mixed small and large cell or diffuse large cell categories. Several of the more common PTCLs are discussed in greater detail below.
Peripheral T-cell Lymphomas Not Otherwise Specified (PTCL-NOS)

Note in the center a large, polylobated cell with moderate amounts of pink to clear cytoplasm. |
True to their T-cellish nature, PTCL-NOSs (image) initially involve a lymph node in the paracortex and never grow in a true follicular pattern. Four other features often though not always seen are:
- An admixture of non-neoplastic
inflammatory cells, including plasma cell, eosinophils, epithelioid histiocytes, and others. This benign component is more frequently seen in lower grade lymphomas, where some of the malignant T-cells remember how to make cytokines.
- Cytoplasm that is moderate or abundant in amount and may be pale or
clear.
- Nuclear outlines that are convoluted rather than cleaved.
- Increased vascularity.
The cells often display a range of atypia, with large, atypical forms more frequent in the higher grade cases. The lymphomas home to retroperitoneal sites more commonly than mediastinal ones; and visceral organs and skin, but not the peripheral blood, are also commonly affected. Unlike mycosis fungoides, skin involvement usually spares the epidermis.
Patients, who are mainly adults, usually present with advanced, stage IV lymphoma. A minority of patients will have evidence of prior auto-immune disease. Earlier studies indicated that PTCL-NOSs were diffuse, aggressive lymphomas prognostically like their B-cell counterparts with similar morphology. Some later studies, however, predict a worse outcome for patients with T-cell lymphomas.
Immunophenotypically PTCL-NOSs express pan-T-cell antigens. Eighty percent of the lymphomas, however, are immunologically abnormal. One or more T-cell antigen may be aberrantly clonally deleted, of which CD7 is the most common example. In addition, some lymphomas express unnatural combinations of antigens, such as co-expression of CD4 and CD8, or expression of neither. Cases that are clearly lymphomas by morphology are usually branded as T-cell by reactivity for CD2, CD3, CD5, or CD7, or, in paraffin sections, CD45RO (UCHL1), or CD43. The latter, however, may be seen in other hematopoietic neoplasms.
Because this group is morphologically so diverse, multiple examples of PTCL-NOSs are illustrated here:
 T-Cell Hall of Shame T-Cell Hall of Shame  |
| • Case 1: Lymph node with large cell type PTCL. Unusual striped morphology. |
• Case 2A: Skin with minimal PTCL. See 2B for progression. |
• Case 2B: Skin with mixed PTCL. See 2A for earlier invovlement. |
| • Case 3A: Skin with mixed PTCL. See 3B for nodal involvement. |
• Case 3B: Lymph node with mixed PTCL and foci of large cell. See 3A for skin involvement. |
• Case 4A: Skin with PTCL. See 4B for nodal involvement. |
| • Case 4B: Lymph node with PTCL. See 4A for skin involvement. |
• Case 5A: Lymph node with mixed PTCL and foci of large cell. Possibly Lennert's lymphoma. See 5B for marrow involvement. |
• Case 5B: Bone marrow with PTCL. See 5A
for nodal involvement. |
Cutaneous T-Cell Lymphoma
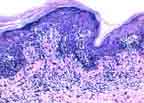 In some circles this phrase denotes any T-cell lymphoma primarily involving the skin. Here, though, the phrase is a synonym for mycosis fungoides (images), which is also called Sezary's syndrome if the malignant lympocytes spill into the
peripheral blood. The charcteristic cell is a medium-sized,
CD4(+) lymphoid cell with a highly cleaved nucleus and darkly clumped chromatin. In the
skin these cells accumulate at the dermal-epidermal junction in a lichenoid infiltrate.
Individual cells drift upward to invade the epidermis without provoking much edema.
Clinically the disease is usually fairly indolent.
In some circles this phrase denotes any T-cell lymphoma primarily involving the skin. Here, though, the phrase is a synonym for mycosis fungoides (images), which is also called Sezary's syndrome if the malignant lympocytes spill into the
peripheral blood. The charcteristic cell is a medium-sized,
CD4(+) lymphoid cell with a highly cleaved nucleus and darkly clumped chromatin. In the
skin these cells accumulate at the dermal-epidermal junction in a lichenoid infiltrate.
Individual cells drift upward to invade the epidermis without provoking much edema.
Clinically the disease is usually fairly indolent.
Skin involvement may go through
patch, plaque, tumor, and generalized erythroderma stages. Lymph node, blood, or
visceral involvement is a bad sign. If the skin disease is minimal, it may be
bafflingly difficult to distinguish the lymphoma from inflammatory conditions,
which on occasion may even yield signs of clonality.
Anaplastic Large Cell Lymphomas (ALCL)
 So-called "classic" ALCL (images) is most common in children and adolescents, often involves the
skin, and has a high frequency of translocation t(2;5). Primary cutaneous ALCL tends to
occur more in adults and lacks the translocation. The characteristic cell has large, often
lobated, open nuclei, which may be multiple and assume a wreath-like configuration in the cell
periphery. Individual nuclei have also been described as embryoid. Nucleoli are present
but not prominent.
So-called "classic" ALCL (images) is most common in children and adolescents, often involves the
skin, and has a high frequency of translocation t(2;5). Primary cutaneous ALCL tends to
occur more in adults and lacks the translocation. The characteristic cell has large, often
lobated, open nuclei, which may be multiple and assume a wreath-like configuration in the cell
periphery. Individual nuclei have also been described as embryoid. Nucleoli are present
but not prominent.
The cells are reactive for CD30 and usually other T-cell markers.
Less commonly they are reactive for B-cell markers, and occasionally an ALCL may lack
lineage-specific features. In lymph nodes the malignant cells tend to expand the sinuses
and to occur in clusters. This low power mimicry of carcinoma is
rendered more treacherous by immunophenotypic mimicry as well--occasional ALCLs may be:
 • (-) for LCA (leukocyte common antigen, a pan-lymphoid marker). • (-) for LCA (leukocyte common antigen, a pan-lymphoid marker).
 • (-) for B- and T-cell markers. • (-) for B- and T-cell markers.
 • (+) for EMA (epithelial membrane antigen, usually present on epithelial cells). • (+) for EMA (epithelial membrane antigen, usually present on epithelial cells).
Worst of all, uncommonly ALCLs may be (+) for keratin--a set-up for the unwary pathologist to make a misdiagnosis of carcinoma.
Despite the very atypical morphology, these lymphomas may have a better prognosis than their more aggressive cousins, with an overall survival rate of 50-60%.

Table of Contents |
Next section |
Previous section
|


