
Go to:

TOC
Prev
Next
|
High Grade B-Cell Lymphomas
COMPARED to intermediate grade lymphomas, high grade lymphomas behave more aggressively, require more intensive chemotherapy and occur more often in children. Because
rapidly dividing cells are more sensitive to anti-cancer agents
and because the young patients usually lack other health problems, some
of these lymphomas show a dramatic response to therapy.
The Working Formulation classifies 3 types of high grade
lymphomas: immunoblastic, lymphoblastic and small non-cleaved cell lymphoma.
Immunoblastic lymphomas were included in the discussion of intermediate
grade lymphomas, where clinical experience has shown they best fit. Lymphoblastic
lymphomas are usually T-cell processes; but in order to compare and contrast
them with B-cell lymphomas, they will be covered in this section.
Lymphoblastic Lymphoma
These lymphomas (images) occur mainly in children and adolescents, where
they account for about half of pediatric lymphomas. About two-thirds of
the patients are males. A second peak is seen again in patients over 40
years of age. The distinction from acute lymphoblastic leukemia is in part
arbitrary, based on the degree of marrow involvement. The chief biologic
difference is that lymphoblastic leukemias are predominantly
B-cell diseases, unlike the extra-medullary, mostly T-cell lymphoblastic lymphomas. and adolescents, where
they account for about half of pediatric lymphomas. About two-thirds of
the patients are males. A second peak is seen again in patients over 40
years of age. The distinction from acute lymphoblastic leukemia is in part
arbitrary, based on the degree of marrow involvement. The chief biologic
difference is that lymphoblastic leukemias are predominantly
B-cell diseases, unlike the extra-medullary, mostly T-cell lymphoblastic lymphomas.
Lymphoblastic lymphoma usually presents supradiaphragmatically
in the cervical, supraclavicular, and axillary regions. Over half the patients
have an anterior mediastinal mass, which may cause acute chest symptoms.
The marrow is focally involved in about half the cases, and other extranodal
sites are common. Spread to the gonads or central nervous system is especially
significant because in these "privileged" hideouts the lymphoma
finds sanctuary from the usual chemotherapeutic agents.
Untreated patients do dismally. With intensive
chemotherapy, however, long-term disease-free survival may be attained,
and the childhood complete remission rate is as high as 96%.
 Lymphoblastic lymphoma cells are larger than benign
lymphocytes but smaller than histiocytes. The nuclei are convoluted or
regular in contour and contain finely granular, dark chromatin and at most
inconspicuous nucleoli. The lymphoma often extends into perinodal soft
tissue. It may display the "starry-sky" pattern more usually associated
with Burkitt's lymphoma. The cells are called "blasts" because
they are the neoplastic counterpart of normal thymic or marrow early lymphoid
precursors, which have never seen antigen. Thus they differ from
the "centroblasts" and "immunoblasts" of intermediate
grade lymphomas, which correspond to normal cells undergoing a second round
of proliferation in response to antigen stimulation. Lymphoblastic lymphoma cells are larger than benign
lymphocytes but smaller than histiocytes. The nuclei are convoluted or
regular in contour and contain finely granular, dark chromatin and at most
inconspicuous nucleoli. The lymphoma often extends into perinodal soft
tissue. It may display the "starry-sky" pattern more usually associated
with Burkitt's lymphoma. The cells are called "blasts" because
they are the neoplastic counterpart of normal thymic or marrow early lymphoid
precursors, which have never seen antigen. Thus they differ from
the "centroblasts" and "immunoblasts" of intermediate
grade lymphomas, which correspond to normal cells undergoing a second round
of proliferation in response to antigen stimulation.
Lymphoblastic lymphoma cells
contain nuclear terminal deoxynucleotidyl transferase (Tdt). This is appropriate
for an early lymphoid cell, which requires that enzyme to rearrange its
immune genes. About 80% of lymphoblastic lymphomas are T-lineage. These
display the earliest T-cell markers CD7 and CD2 in addition to later
markers depending on the lymphoma's maturity. B-cell lymphoblastic
lymphomas usually express B-cell marker CD19 and most also react for CD10
(called CALLA: common acute lymphoblastic leukemia antigen). They
do not express surface immunoglobulin. Testing for Tdt and these other markers is
part of working up a new lymphoblastic lymphoma.
Small Non-Cleaved Cell
Lymphoma
Small non-cleaved cell lymphoma (SNCL) comes (images) in 3 varieties, all of which are more prevalent in males:
-
Endemic Burkitt's lymphoma: a childhood lymphoma prevalent in equatorial
Africa and intimately associated with both Epstein-Barr virus infection
and a characteristic translocation of the MYC gene.
-
Sporadic Burkitt's lymphoma: a world-wide lymphoma affecting slightly older
patients, also associated with MYC changes but less so with
EBV infection.
-
Non-Burkitt's lymphoma: a rather different disease affecting
an older population and not notably associated with the MYC gene
or EBV infection.
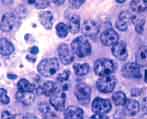 The morphology of endemic and sporadic Burkitt's is the same: expansile
sheets of monotonous, fiercely mitotic cells with nuclei the size of histiocyte
nuclei. The chromatin is coarse, and the multiple nucleoli are prominent.
On smears, the amphophilic cytoplasm includes numerous
lipid-laden cytoplasmic vacuoles. Scattered tingible-body macrophages (histiocytes with fragments
of necrotic lymphoma cell nuclei in their pale cytoplasm)
stand out in the midst of the dark lymphoma cells, forming a so-called "starry sky"
pattern.
The morphology of endemic and sporadic Burkitt's is the same: expansile
sheets of monotonous, fiercely mitotic cells with nuclei the size of histiocyte
nuclei. The chromatin is coarse, and the multiple nucleoli are prominent.
On smears, the amphophilic cytoplasm includes numerous
lipid-laden cytoplasmic vacuoles. Scattered tingible-body macrophages (histiocytes with fragments
of necrotic lymphoma cell nuclei in their pale cytoplasm)
stand out in the midst of the dark lymphoma cells, forming a so-called "starry sky"
pattern.
The poor prognosis of endemic Burkitt's lymphoma is tied to its occurrence mainly
in under-developed countries with less sophisticated medical facilities.
Both sporadic Burkitt's and non-Burkitt's lymphoma behave similarly: untreated
they are extremely aggressive. Both diseases, however, may respond well
to intensive chemotherapy. Small non-cleaved cell lymphoma is one of
the most common types of lymphoma seen in patients with AIDS.
The following table compares and contrasts features of these 3 types
of small non-cleaved cell lymphoma. |


